FAQS
Facts About Neuroendocrine Carcinoma of the CervixHigh-grade Neuroendocrine Cervical Cancer (Small and Large cell) FAQ
Disclaimer: The purpose of this frequently asked questions (FAQ) is to promote broad patient and family member understanding and knowledge of neuroendocrine cervical cancer. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of information you have read on this website.
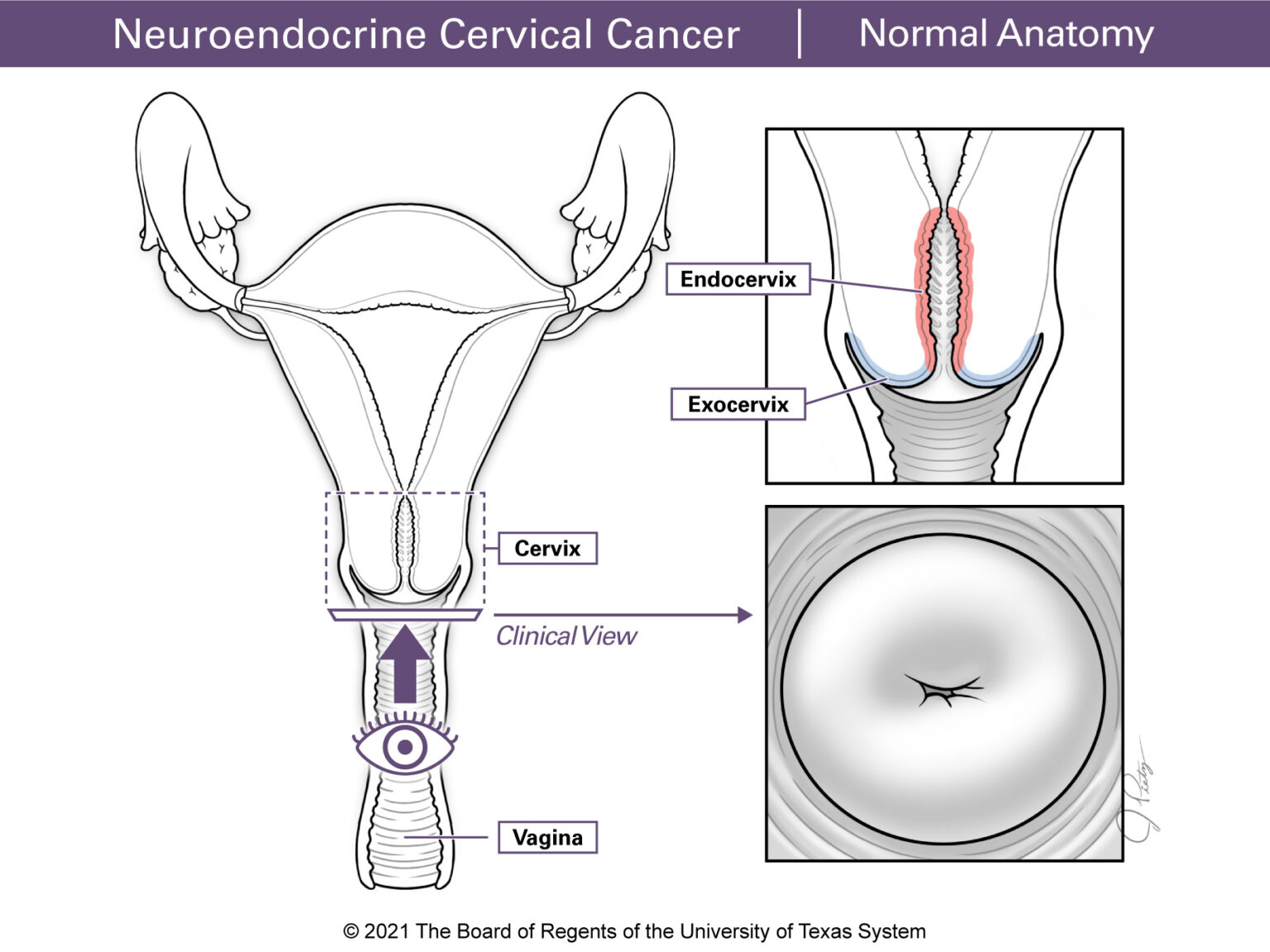
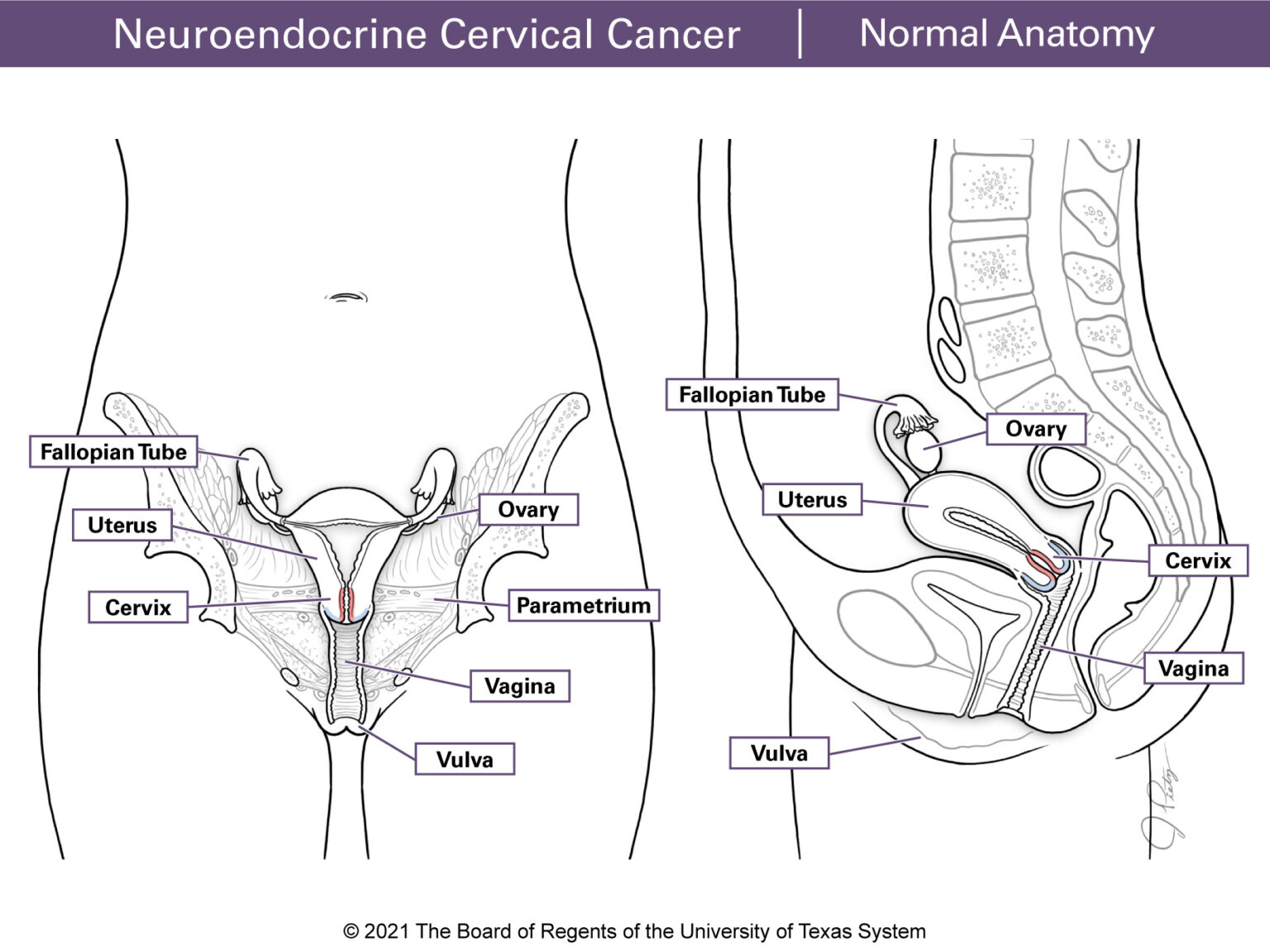
The cervix is the lower, narrow end of the uterus. It is a 3 to 4 cm cylinder-shaped structure that plays a critical role in female reproduction. The cervix connects the uterus to the vagina. (Figure 1 & Figure 2) The lining of the cervix has glands that make mucus which changes during the menstrual cycle. Around ovulation the mucus is thin, which allows sperm to pass into the uterus. The uterus connects to the fallopian tubes. For most of the menstrual cycle and during pregnancy the mucus is thick. This helps prevent infections from entering the internal reproductive organs (vagina, uterus, fallopian tubes, and ovaries). During childbirth, the cervix widens and opens (dilates), which allows the baby to pass through the birth canal.
The cervix has 2 parts:
- The endocervix is the inner part of the cervix (the canal leading into the uterus) with a small opening into the vagina.
- The ectocervix (or exocervix) is the outer part of the cervix. It is rounded in shape and has tissue that forms a lip that goes into the vagina.
Surrounding the cervix there is a fibrous structure called parametrium that helps connect the cervix to other tissues in the pelvis.
Cervical Cancer
Cervical cancer is a disease in which cancer cells grows in the cells of the cervix.
Most cervical cancers are either squamous cell, adenocarcinoma or less often, adenosquamous. They often develop from precancerous changes in the cervix. Most of these changes are caused by a long-term infection with the human papillomavirus (HPV). Most precancerous changes in the cervix do not progress to cancer. When they do, it often takes several years for cancer to develop.
- The neuroendocrine system is made up of neuroendocrine cells. These cells are found throughout the body but are mainly in the intestines, pancreas, thyroid and lungs. Neuroendocrine cells are also located in the thymus, kidneys, liver, prostate, skin, cervix, ovaries and testicles. These cells are like nerve cells (neurons), but they also make hormones like other types of endocrine cells. They receive messages (signals) from the nervous system and respond by making and releasing hormones. These hormones control many body functions. Neuroendocrine tumors start in cells of the neuroendocrine system. They are classified as functional or non-functional.
- Functional tumors make too much of a certain hormone and often cause symptoms related to the extra hormones in the body. Non-functional tumors do not usually cause any symptoms. Neuroendocrine tumors are rare in the female genital tract. Cervical neuroendocrine cancer that start in the neuroendocrine cells of the endo- or ectocervix usually are non-functional and are very rare.
Neuroendocrine cervical carcinoma (NECC) is divided into 3 categories:
- Low-grade neuroendocrine tumors (also called carcinoid or atypical carcinoid tumors)
- High-grade neuroendocrine tumors (also called small-cell carcinoma and large-cell neuroendocrine carcinoma)
- Adenocarcinoma are mixed with neuroendocrine carcinoma tumors
In the cervix, high-grade (small and/or large cell) neuroendocrine cancer is the most common.
It is also common to see mixed tumors. These are high-grade neuroendocrine tumors (small and/or large cell) mixed with adenocarcinomas. Sometimes they are seen with squamous cell tumors. Mixed small and large cell tumors can also be found together as well.
With squamous cell carcinoma or adenocarcinomas, HPV infection is often the main cause of these cervical cancers. There may also be other factors or causes. A long-term infection of HPV can develop into pre-cancer of the cervix. After several years, this may become cervical cancer. Studies now show there is a strong connection between neuroendocrine cervical tumors, HPV and cancer.
Staging describes cancer based on the size and amount of the disease. Cancers are staged at the time of diagnosis and do not change during treatment or recurrence.
Cervical cancer is staged as I to IV (1 to 4). To determine the stage, a physical exam is done. This includes looking at the cervix and doing a pelvic exam. During the exam the doctor checks your cervix, uterus and ovaries. This is done with a gloved hand and placing a finger or two in your vagina and the other hand on your lower stomach. This is one way to check if a tumor extends into your vagina or nearby tissues. A rectovaginal exam is also done to check if the tumor has spread to the parametrium (the tissue that connects the cervix to other pelvic structures). The rectovaginal exam is done with a gloved hand with a finger placed in your anus. Many neuroendocrine tumors start from the endocervical canal. Often, these tumors are not visible when using a speculum. This is because the ectocervix, which is what the doctor can see, can look completely normal. Imaging studies such as an MRI or a pelvic ultrasound may also be used to check for local spread of cervical cancer.
If a patient is a candidate for surgery (the tumor is only in the cervix), the final results of the pathology from tissue taken during surgery also helps to determine the stage. The stage of cancer may change from the original stage at diagnosis. This may happen if the tumor (removed during surgery) was larger than expected, or in the tissues of the parametrium or if it was found in nearby lymph nodes. These may not always be visible on the images taken before surgery.
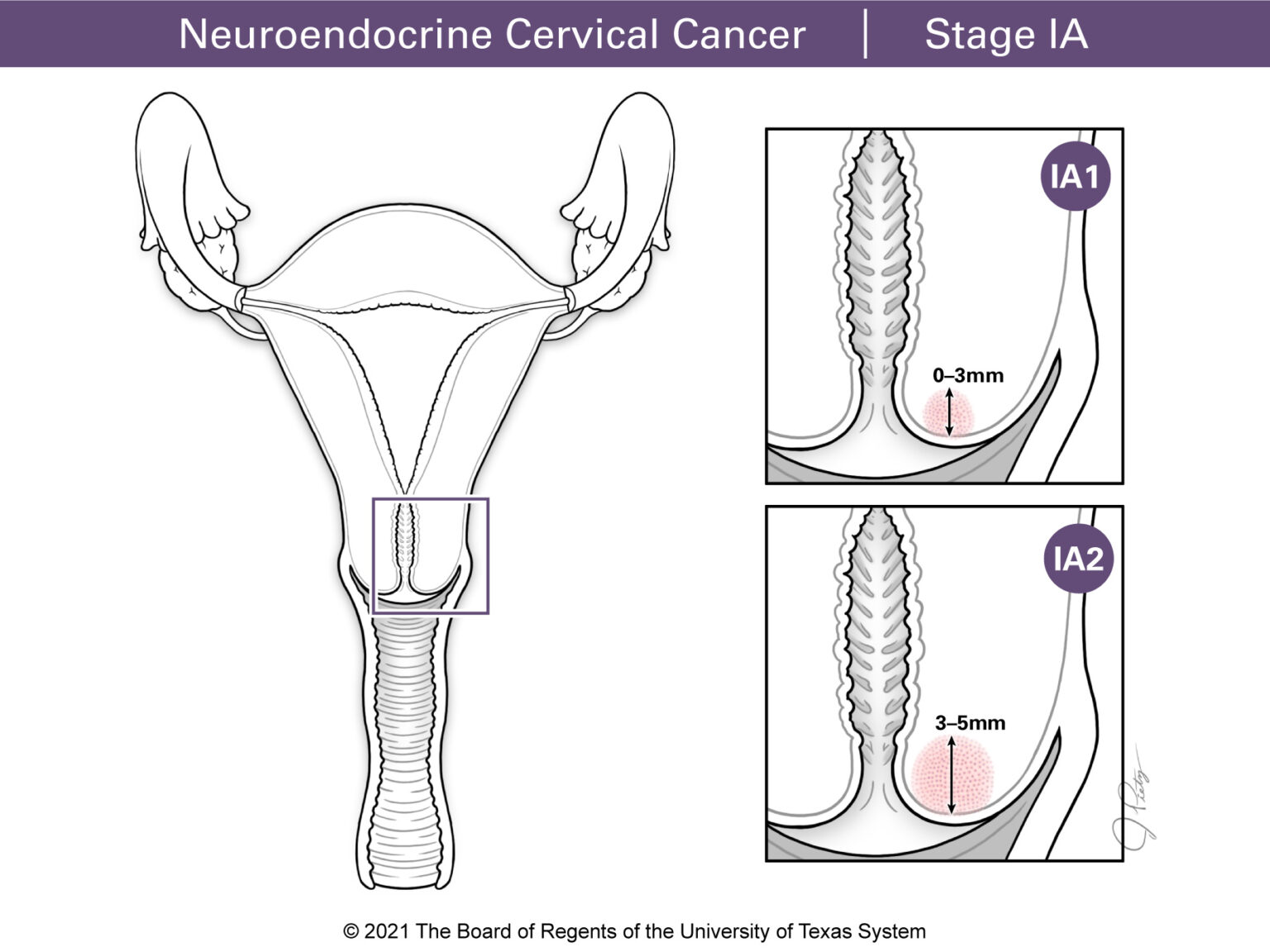
Stage I
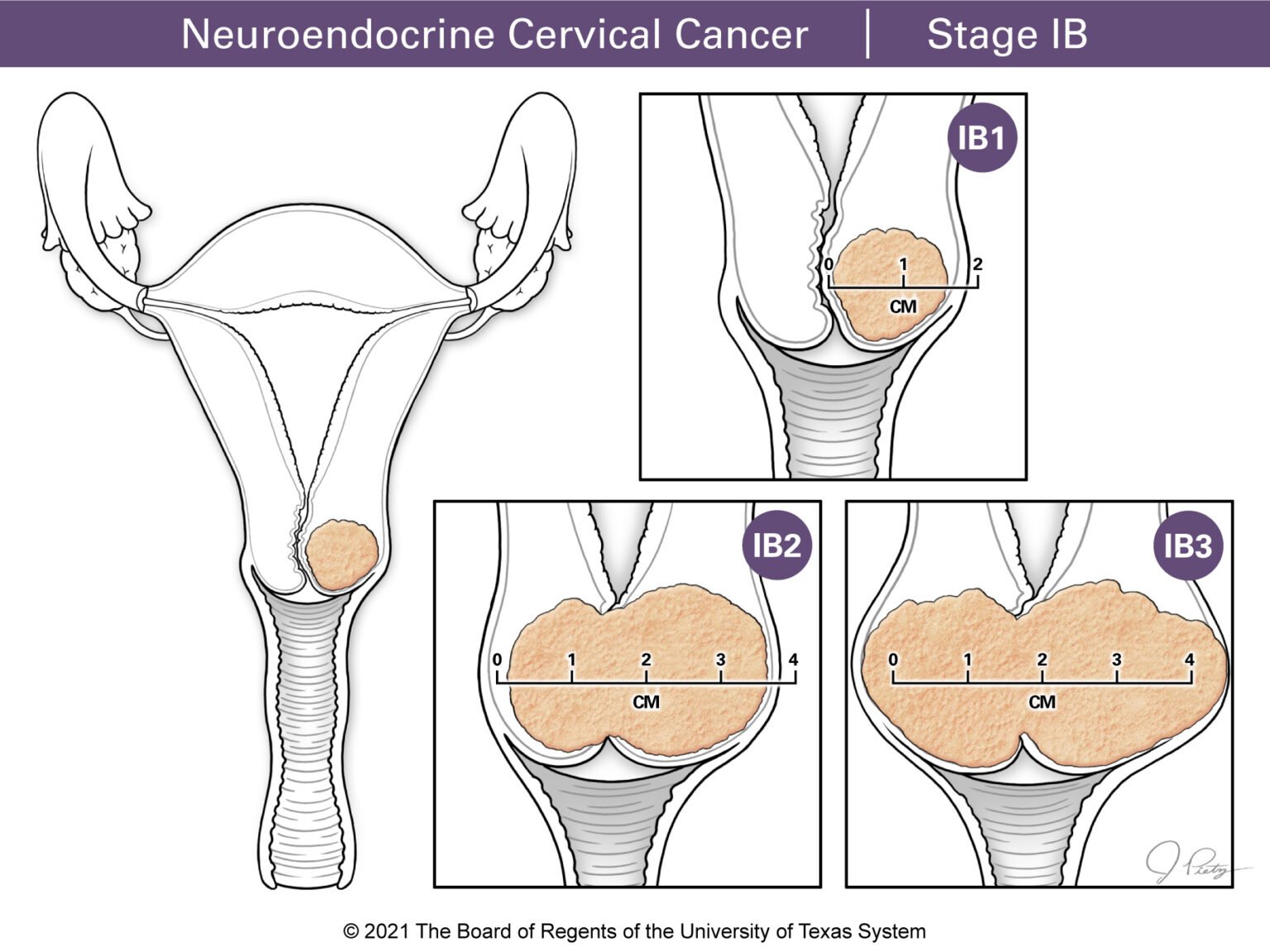
Stage I means the tumor is only in the cervix. Categories under Stage I include Stages IA1 and IA2 for tumors that can only be seen under a microscope and
Stages IB1, IB2 or IB3 for tumors that can be seen by the naked eye.
Stage II
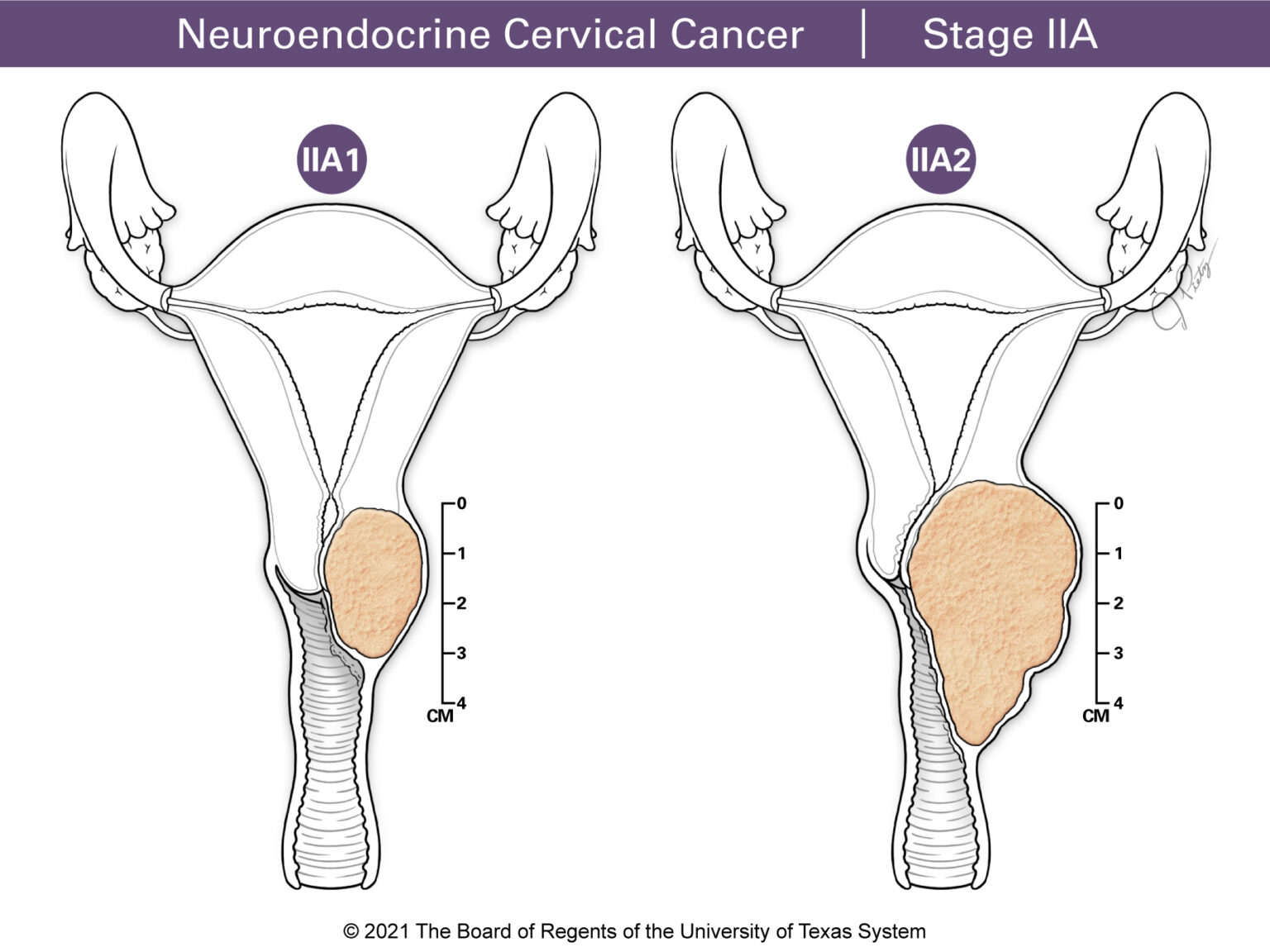
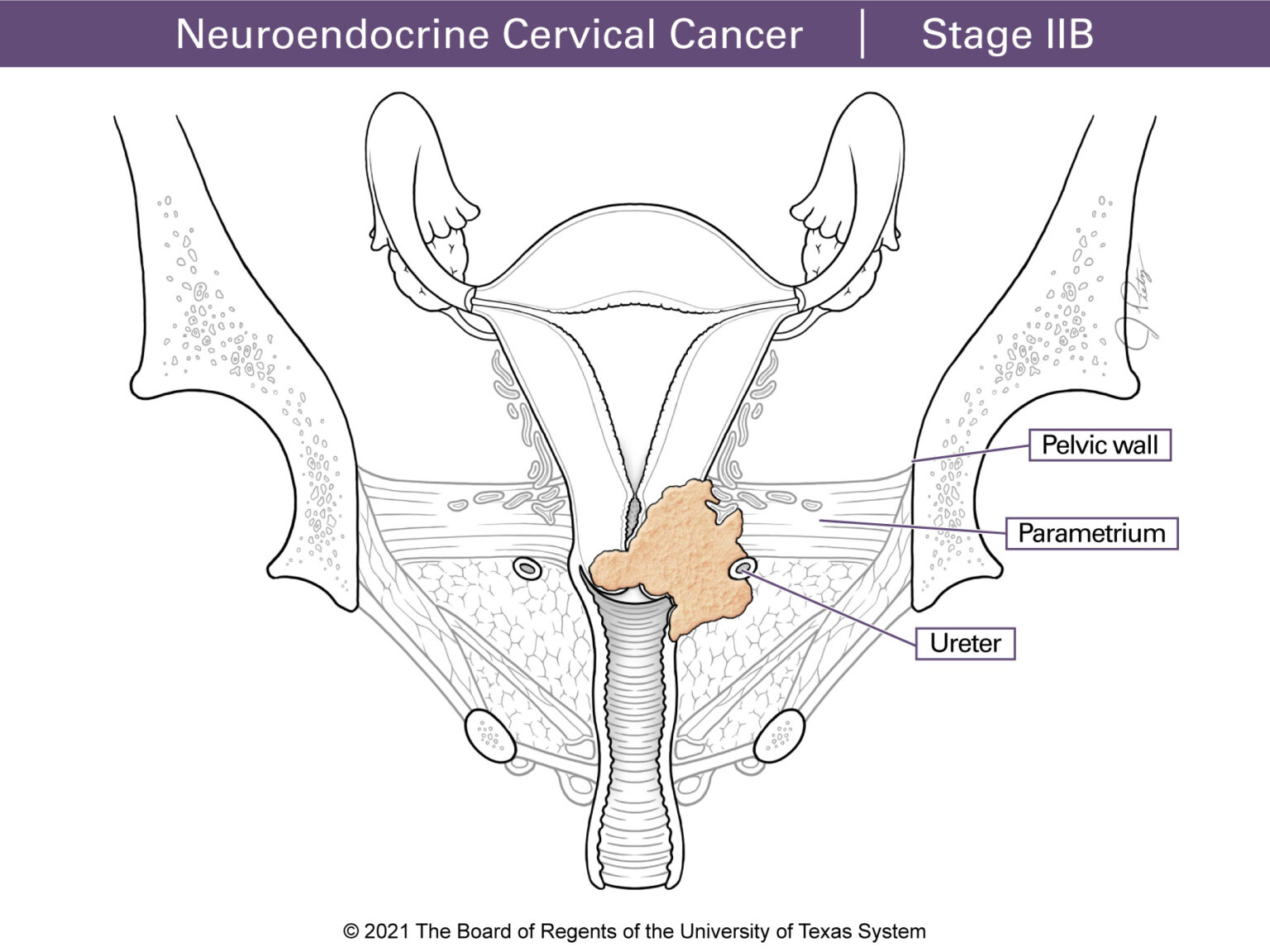
Stage II means the tumor extends past the cervix. Stage IIA involves the upper part of the vagina and Stage IIB includes the tissues of the parametrium.
Stage III
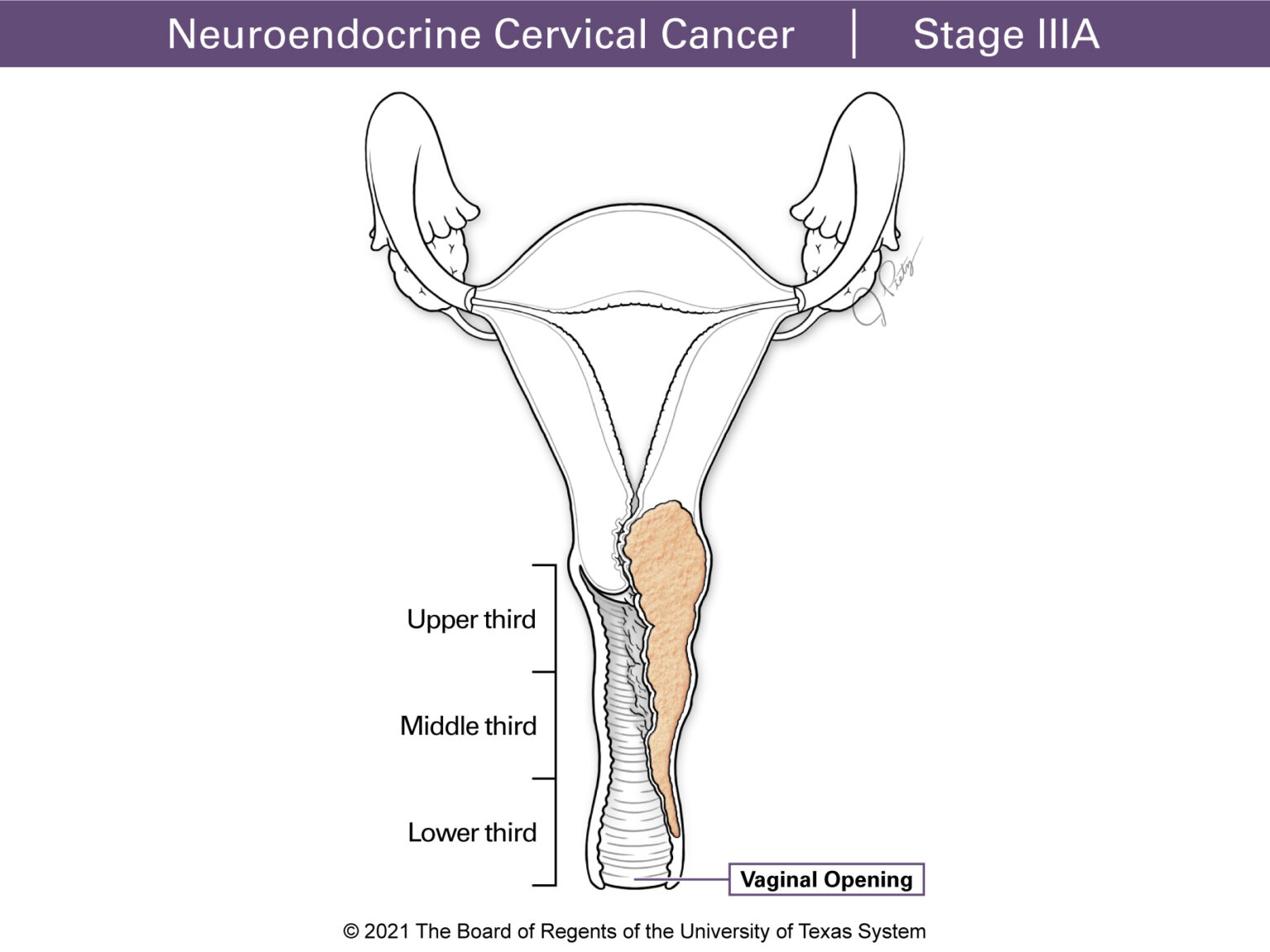
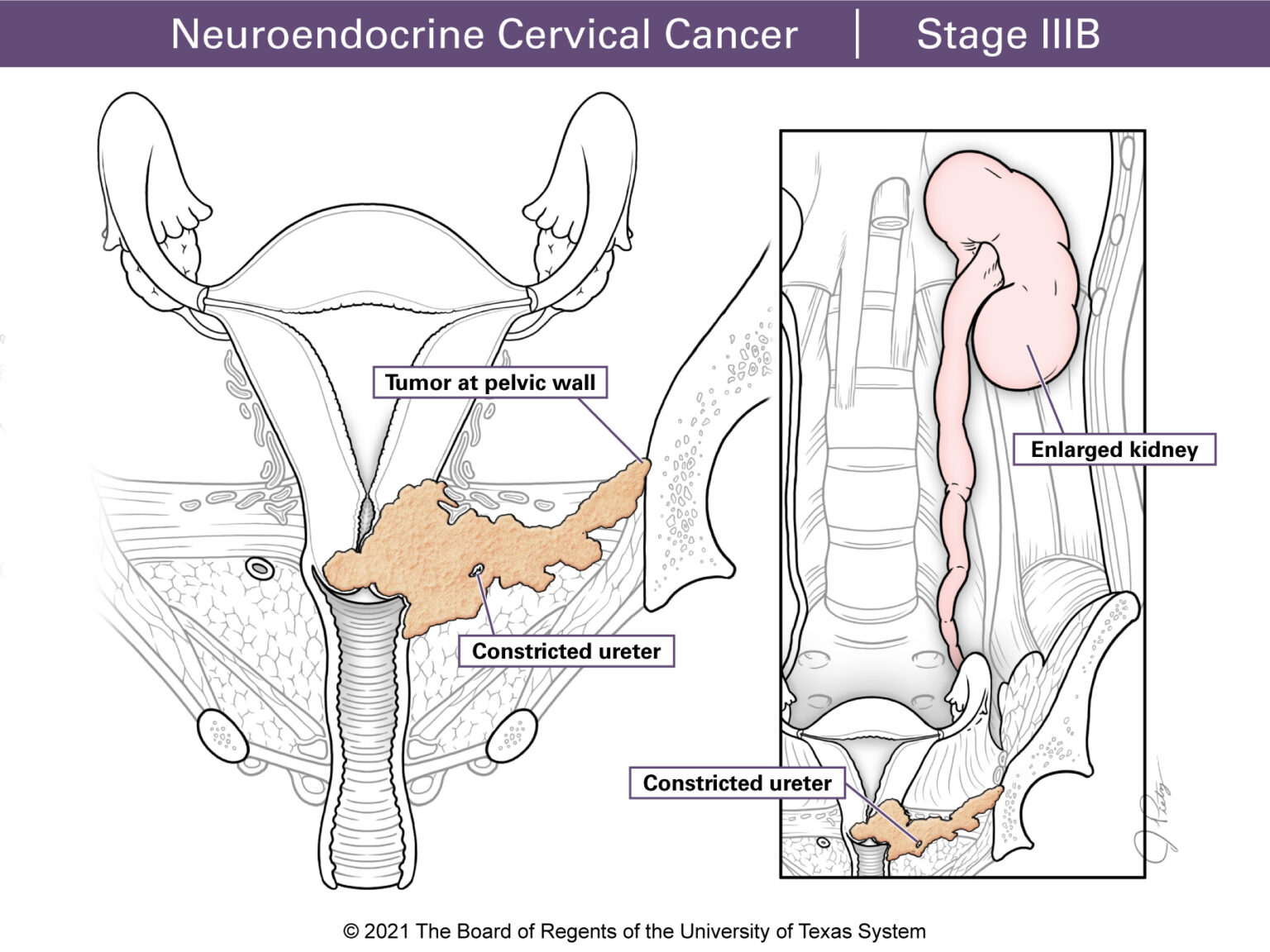
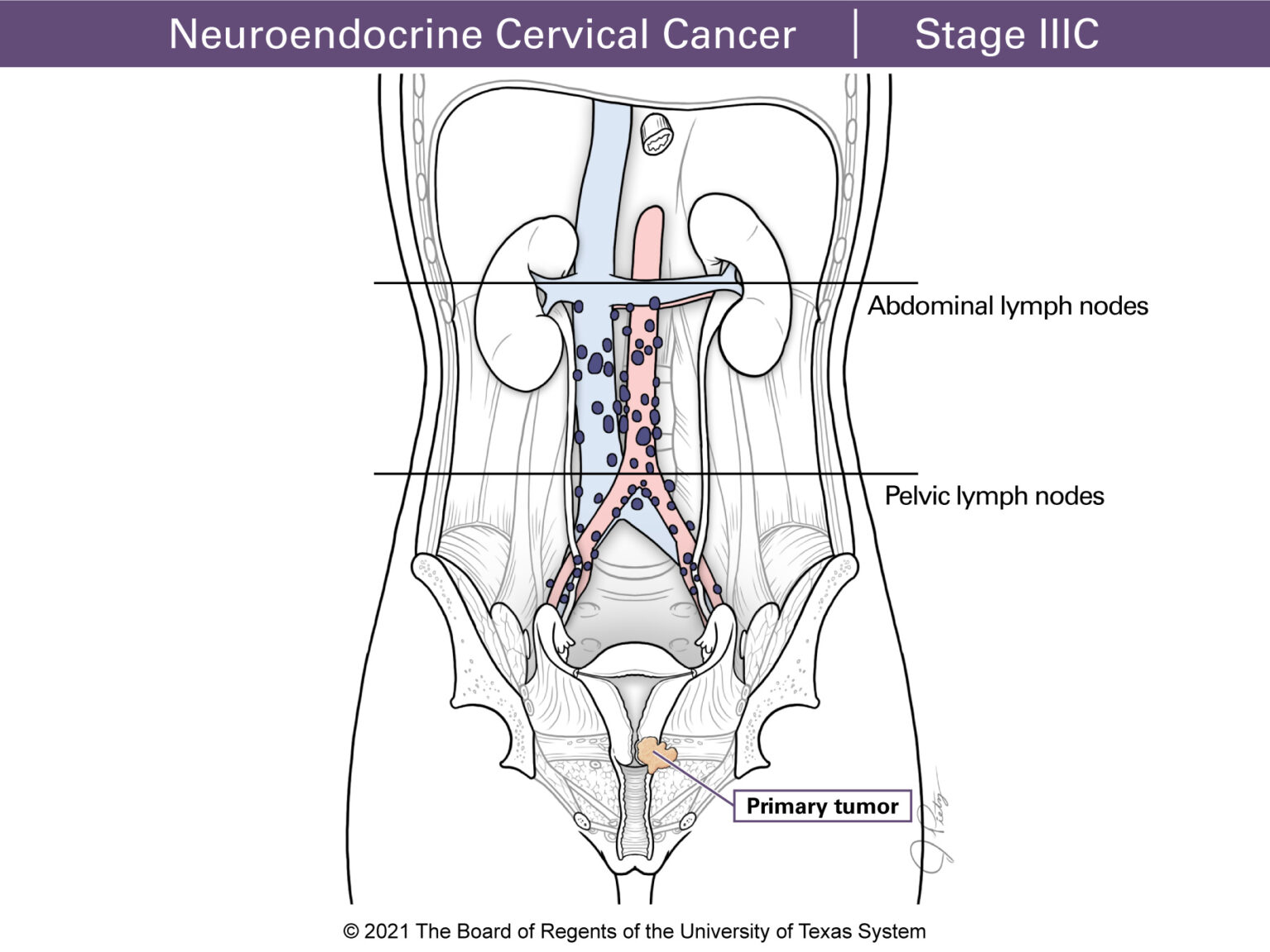
Stage III tumors have grown past your upper vagina or parametrium. Stage IIIA means the tumor has reached the lower part of the vagina. Stage IIIB involves the parametrium and the pelvic wall. When this happens urine can back up to the kidneys. This is called hydronephrosis and defines Stage IIIB. Stage IIIC means the cancer has reached the lymph nodes. Stage IIIC1 means the cancer has spread to the pelvic lymph nodes, and StageIIIC2 means the lymph nodes around the large blood vessel in the pelvis (paraaortic) are involved.
Stage IV
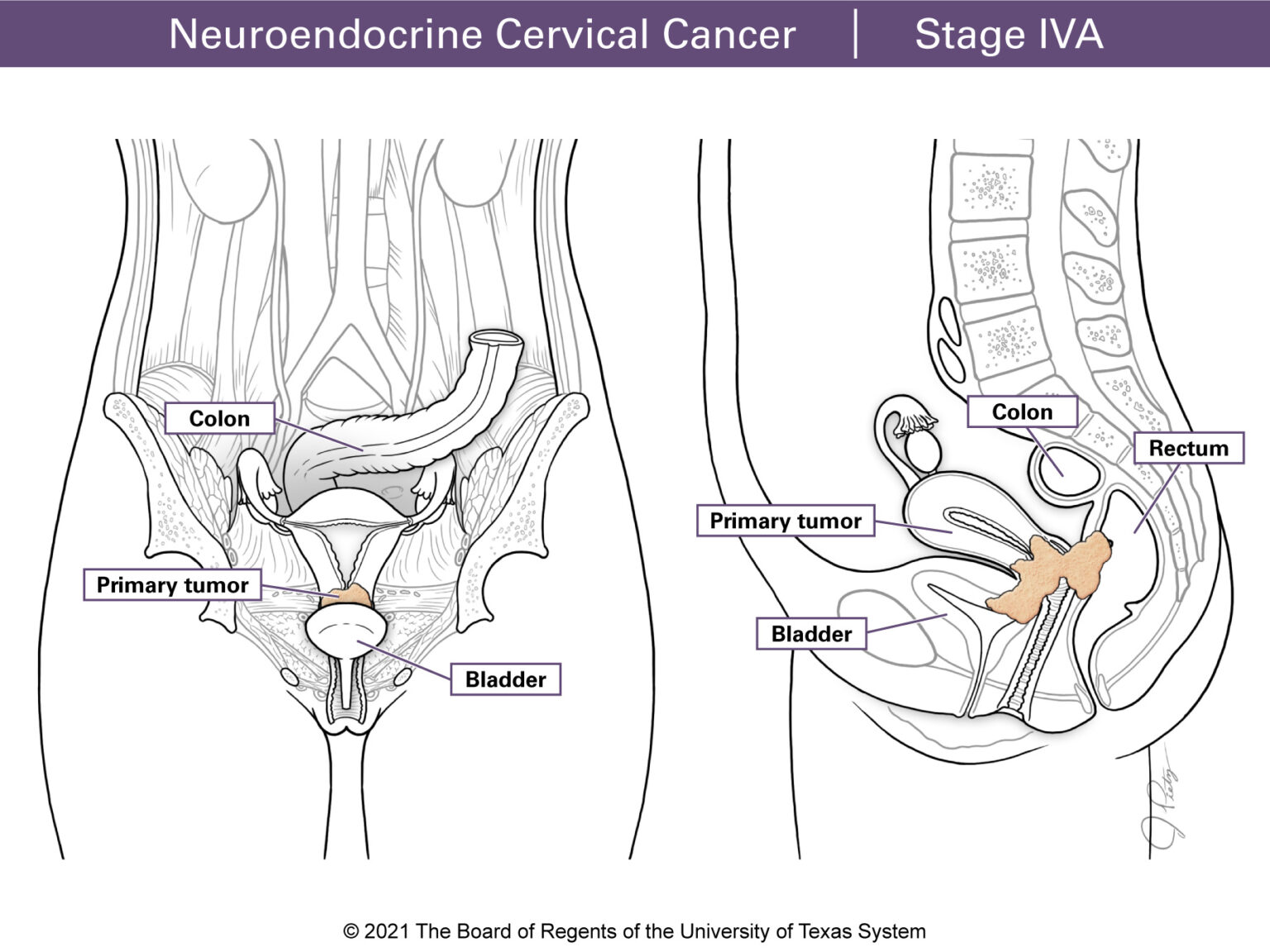
Stage IVA tumors have spread (metastasized) to other pelvic organs such as the bladder or rectum.
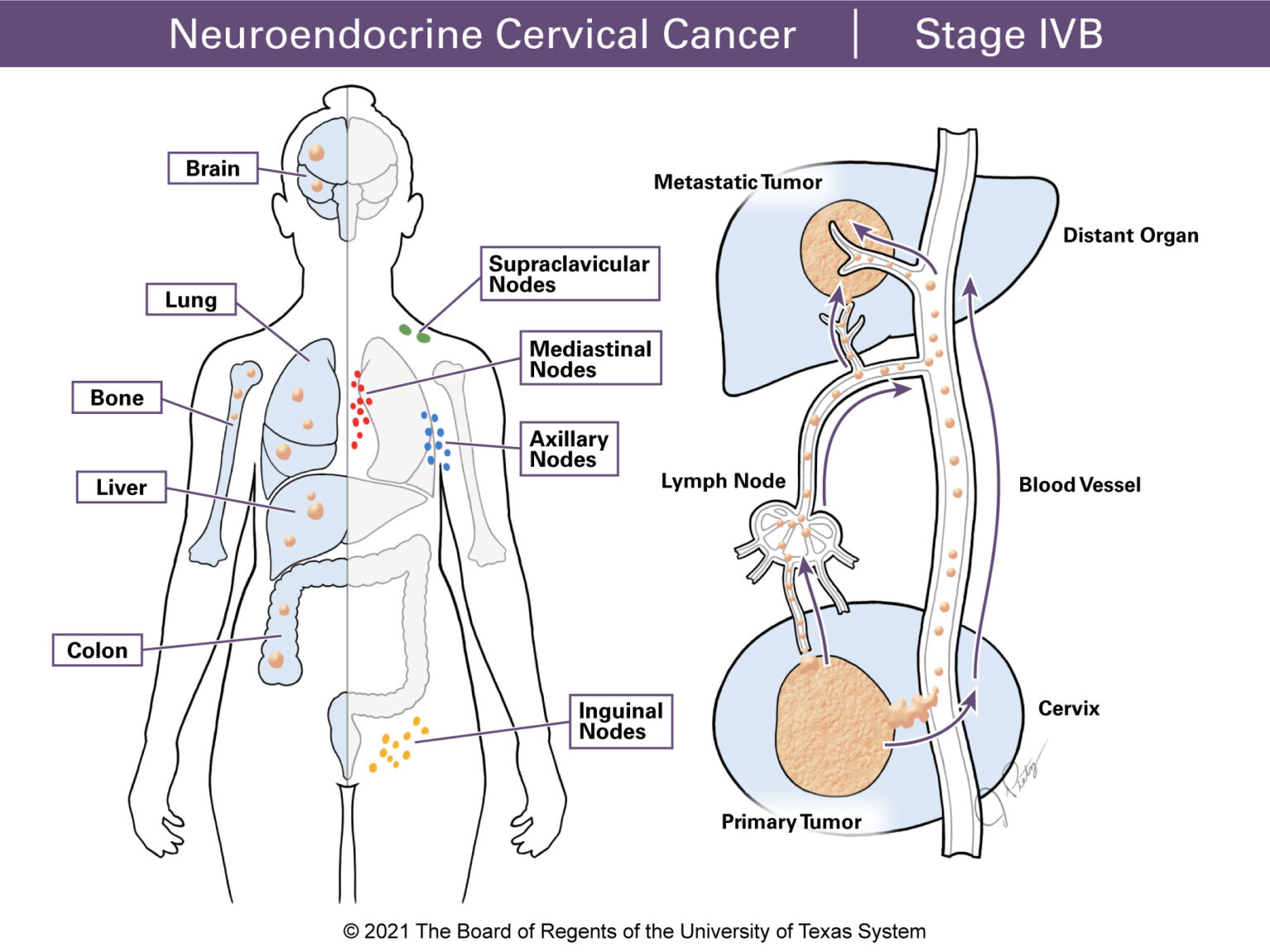
Stage IVB tumors have spread to distant organs. This may include the lungs, liver or brain. In addition, the cancer may have spread to distant lymph nodes such as the supraclavicular, axillary, inguinal or mediastinal nodes.
Tumor staging allows doctors to choose the best treatment options. All stages are not treated in the same way. Stage also helps to understand outcome. In general, an early stage cancer may have a better outcome than an advanced stage cancer.
Neuroendocrine tumors are staged using the same system as other cervical cancer types. These tumors are often found in other parts of the body at diagnosis. A PET/CT or a CT scan (which includes the chest, abdomen and pelvis) is often performed at diagnosis to rule out the spread to other parts of the body.
Different stages can be grouped into categories according to treatment options. For cervical cancer, they can be divided into early, locally advanced, and advanced stage.
- Early-stage tumors are up to 4 cm in size and are in the cervix or upper vagina. They include Stages IA1, IA2, IB1, IB2 and IIA1. Sometimes some may include Stage IIA1 as locally advanced. The FIGO classification system considers the pathology report (from the surgical tissue examined by the pathologist) as part of the staging. This means that a patient can be staged as Stage IIB or IIIC1 due to microscopic disease found in the parametrium or pelvic nodes.
- Locally advanced tumor includes Stages IB3, IIA2, IIB, IIIA, IIIC1, IIIC2 and IVA. These tumors are bigger in size and go beyond the cervix affecting the nearby pelvic structures. Surgery is usually not an option for this type of tumor. This is because the tumor goes past the tissue that can be removed with surgery, which would leave some of the tumor in the pelvis.
- Advanced stage tumors include Stage IVB where the tumor has spread to distant organ(s) through the lymphatic system (to distant lymph nodes as supraclavicular, mediastinal, axillary) or blood vessels (to the liver, lungs, bones). For this stage surgery is not an option and patients are usually treated with chemotherapy such as cisplatin or carboplatin and etoposide. Radiation therapy is often used to ease symptoms such as vaginal bleeding.
Primary treatment is the first treatment a patient receives after diagnosis. It may be surgery alone, surgery followed by radiation and/or chemotherapy, chemotherapy + radiation followed by more chemotherapy or chemotherapy alone depending on the stage.
For tumors up to 4 cm with negative lymph nodes and parametrium (on pre-operative exam and imaging), the first treatment option is surgery and removal of lymph nodes for biopsy.
After surgery, chemotherapy + radiation followed by chemotherapy is recommended. The goal is for patients to receive a total of 6 cycles of chemotherapy.
No. Radiation to the brain or head is not often recommended as a preventive measure for women with high-grade neuroendocrine cervical cancer.
For women with Stages IB3-IVA cancer or those who are not able to have surgery, the recommendation is chemotherapy (cisplatin and etoposide) + radiation followed by more chemotherapy with cisplatin and etoposide, for a total of 5 to 6 cycles (2 to 3 cycles with radiation and 3 to 4 cycles after radiation is completed) with a goal of at least 5 cycles total.
For women with Stage IVB cancer, chemotherapy with cisplatin and etoposide is recommended. Radiation therapy to the pelvis might be an option to ease symptoms often seen in this stage of the disease.
The follow up plan includes a physical and pelvic exam every 3 to 4 months for the first 2 years, followed by every 4 to 6 months for the next 3 years. In addition, routine imaging of the chest, abdomen and pelvis, with either a CT scan or PET/CT scan is done at every visit.
On average, 61 out of 100 (61%) women with early-stage neuroendocrine cervical cancer live 5 years after diagnosis.
On average, 27 out of 100 (27%) women with advanced stage cancer live 5 years after diagnosis.
On average, 12 out of 100 (12%) women with advanced stage cancer live 5 years after diagnosis.
Symptoms of menopause are a major health concern after treatment for cervical cancers. Menopause symptoms may result from the removal of both ovaries, chemotherapy and/or pelvic radiation. Not all menopausal symptoms need treatment. Cancer patients may have more severe symptoms compared to women going through natural menopause.
Menopause symptoms may include:
- Night sweats
- Hot flashes
- Vaginal dryness or discomfort
- Pain with intercourse or sexual activity
- Bone loss, (osteopenia, osteoporosis)
- Confusion or memory loss
- Increased risk of heart disease.
For premenopausal women who have surgery, saving the ovaries – one or both (called ovarian conservation) may be an option if no tumor is seen by the naked eye, during surgery.
For patients who have chemoradiation therapy either after surgery or as their primary treatment, ovarian transposition aims to lessen the amount of damage and exposure of radiation to the ovaries. This is a done with a procedure where one or both ovaries are separated from the uterus and moved away from the area where radiation is delivered. Ovarian function may be preserved with this procedure.
Women who have early, or premature menopause should be offered hormone replacement therapy (HRT). This therapy should be taken until the average age of natural menopause (around age 51). It helps manage symptoms and lessen bone loss linked to early loss of natural estrogen. Women who had a hysterectomy can be offered estrogen-only therapy. Women who still have their uterus need both estrogen and progesterone. HRT is the most effective treatment for symptoms. HRT can be taken by mouth or through the skin with a patch. For women who have vaginal dryness and discomfort, vaginal estrogens may help symptoms. After radiation to the pelvis, vaginal dilators with topical estrogen cream may help prevent vaginal narrowing and scar tissue.
HRT for women who have menopause due to treatment is safe and often recommended for patients under 50 years old.
A gene mutation is a permanent change or damage to the DNA that makes up a gene. The 2 major categories of mutations are germline and somatic.
- Hereditary or germline mutations are inherited from a parent and are present throughout a person’s life in every cell in the body.
- Acquired or somatic mutations occur at some time during a person’s life and are present only in certain cells either due to mistakes when the DNA is copied or as the result of environmental factors such as UV light or cigarette smoke. Acquired mutations in somatic cells (cells other than sperm and egg cells) cannot be passed to the next generation.
High-grade neuroendocrine cancer of the cervix almost always develops as a result of somatic mutations. There are no known inherited mutations that put women at risk for this type of cancer. All cancer is the result of gene mutations. Mutations may be caused by aging, exposure to chemicals, radiation or other factors in the body or the environment. Over time, a number of mutations may occur in a single cell, which allows it to divide and grow in a way that becomes a cancer.
A mutation test is a test done to find mutations that can be present in a tumor. Identifying these mutations could provide the doctor with information to plan the best treatment. Some medicines can target specific mutations. Mutation tests can be done using tumor tissue (from the biopsy or surgical specimen) or sometimes blood samples (called liquid biopsy) can be used. A mutation test checks for some but not all mutations. New mutations are often identified and added to the tests. This is a growing field in medicine.
When treating patients with recurrent cancer, a tumor mutation test, PD-L1 test and mismatch repair proteins (MLH1, MSH2, MSH6, and PMS2) test are ordered at the time of first recurrence (when the cancer returns).
Mutation tests can be done at any time. Most doctors order them at the time of first recurrence.
In early-stage cancer, almost half (50%) of patients have a recurrence. This percentage is higher for higher stages.
Recurrences can be seen in almost any organ, including the cervix (if it was not removed at primary treatment), other pelvic structures or distant organs. Most recurrences have a distant component. This means that they occur outside the pelvis with the liver and lungs as the most common sites. Other common sites of recurrence include the peritoneum, brain and bones.
Patients may have a recurrence. If recurrence occurs more than 6 months from completing their first therapy, treatment with cisplatin/carboplatin and etoposide can be repeated. If recurrence occurs less than 6 months from completing initial treatment, a chemotherapy regimen which includes 3 medicines (paclitaxel, topotecan and bevacizumab) is a good treatment option.